What is sickle cell disease (SCD)?
Sickle cell disease (SCD) is a group of blood disorders passed from parents to children through genes. It is the most common inherited blood disorder affecting over 100,000 people of all ages in the U.S. It is primarily found in individuals of African, Mediterranean, South American, Southeast Asian, and Middle Eastern descent. SCD causes your body to make unhealthy red blood cells.
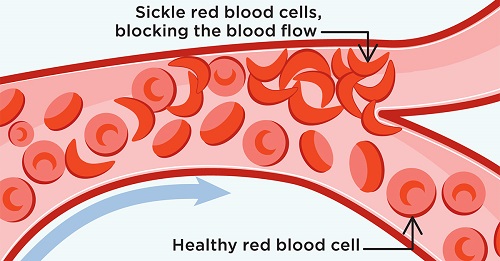
Healthy red blood cells are round and flexible. They move through your small blood vessels and bring oxygen to all parts of your body. With SCD, your red blood cells are misshapen, hard and sticky. They get stuck in your blood vessels and clog them. This can cause you to have pain, infection, organ damage, low blood count, strokes and other serious health problems. This leads to life-long morbidity and reduced life expectancy through end-organ damage.
How does blood or marrow transplant (BMT) work for SCD?
BMT, also known as bone marrow transplant or stem cell transplant, is the only known cure for SCD. It replaces the unhealthy blood-forming cells (stem cells) with healthy ones.
Allogeneic transplant is used for SCD. This type of transplant uses healthy cells donated by someone else to replace the cells that make faulty hemoglobin. These healthy cells can come from a family member, unrelated donor or umbilical cord blood.
First, you get chemotherapy (chemo), to kill the cells that make faulty hemoglobin. Then, the healthy cells are given to you through an intravenous (IV) catheter just like a blood transfusion. The new cells travel to the inside of your bones and begin to make healthy blood cells.
The entire transplant process, from when you start chemo until hospital discharge, can last weeks to months. This is followed by many months of recovery near the transplant center and at home. Your transplant team will closely watch you to prevent and treat any side effects or complications. Transplant doesn’t reverse any organ damage that has already happened, but it can stop more damage from happening.
When should I (or my child) see a transplant doctor?
Sickle cell warriors can request a consultation with a transplant doctor to learn about BMT at any point in their journey. The decision to go to transplant is one that is made between you, your family and your doctors. Transplant may or may not be the best option for you.
For people with an available donor, doctors might recommend transplant if you have any of the following:
- More than 3 severe pain crises within 2 years
- A stroke or silent stroke
- Acute chest syndrome 2 or more times in the last 2 years
- 8 or more red blood cell transfusions per year
- Pulmonary hypertension
- Chronic pain lasting longer than 6 months
- Ultrasounds that show you may be at a high risk for having a stroke
At your first appointment, the transplant doctor will:
- Review your medical history
- Talk with you about your options
- Discuss the risks and benefits of transplant
- Recommend the best time for you to get a transplant and prepare for treatment
- Start a donor search even if you don’t need it right away. This can help you get a transplant faster if it’s needed later.
Questions to ask your doctor
Ask questions so you understand your treatment options and can make decisions that are best for you. You can and should be an active participant in the decision-making process with your care team. Questions you may want to ask:
- Is transplant an option for me?
- What are the chances that transplant will cure my SCD?
- What are the risks of waiting or trying other treatments before transplant?
- Does my age affect the risks of transplant?
- What are the possible side effects of transplant? How can they be reduced?
- How might my quality-of-life change over time, with or without transplant?
Sickle Cell Connect
Learn more about sickle cell disease and transplant and find free resources at SickleCellConnect.com.
